Characterization and Preliminary Research Findings on the Southern Cordilian Novel Pathogen - RK Virus
(Epidemiology, Virology, Molecular Biology, Medicine)
Collated by the Joint Taskforce on RK Virus Vaccine Development
Abstract
A novel pathogen has emerged in Southern Cordilia and parts of Keyli, precipitating a grave public health emergency with confirmed fatalities exceeding 6,000 and widespread infection among vulnerable populations. This paper expands upon initial findings by presenting a more detailed clinical profile of the disease, its transmission characteristics, and virological behavior. The pathogen’s extreme mutability complicates diagnostic efforts and vaccine development. We also analyze the effectiveness of current containment strategies and outline a strategic research agenda for developing long-term immunological solutions.
Keywords: Southern Cordilia, novel virus, outbreak, mutability, systemic infection, cytokine storm, respiratory virus, vaccine development
1. Introduction
Since its emergence in late December 2024, a highly contagious and deadly disease has swept through Southern Cordilia and into Keyli, with epicenters forming in overcrowded refugee camps and conflict-affected urban areas. In response to the accelerating crisis, Krauanagazan and Zuhlgani health authorities formed a joint research taskforce, which now coordinates with international partners in Emerald and Sedunn. This expanded article presents a comprehensive overview of the disease’s biological characteristics, including its clinical syndrome, virology, and implications for regional and global health policy.
2. Epidemiological Overview
The pathogen’s initial transmission vectors were closely linked to dense, unsanitary living conditions in refugee camps in northern Krauanagaz. These populations, already weakened by malnutrition, displacement, and limited access to healthcare, provided fertile ground for the disease to spread rapidly. Current models estimate that 8.3 to 9.1% of the population in affected zones has been exposed.
The disease shows no clear seasonal pattern and spreads rapidly between individuals in both confined and open environments. High-transmission hotspots now include border regions in Eastern Prira, the urban zones of Krautallaz, and military encampments across the Gulf conflict corridor.
3. Clinical Presentation and Disease Progression
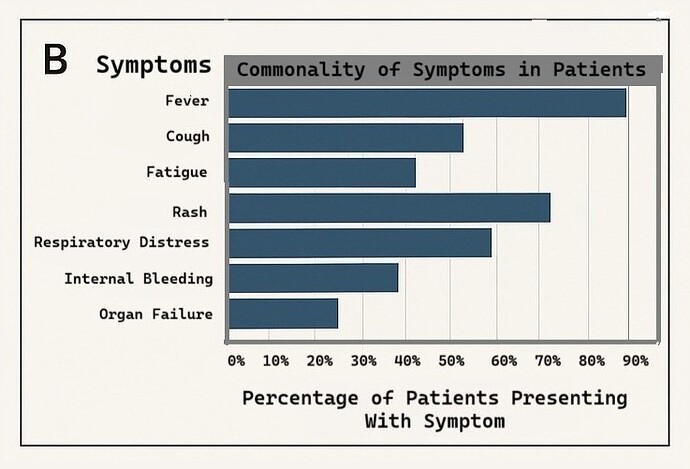
The pathogen causes a multi-stage illness with escalating severity. The average incubation period is 3–5 days. While some asymptomatic carriers exist, the majority of infected individuals experience a progression of the following clinical features:
Early Stage (Day 1–2):
- Sudden onset of high fever (above 39°C/102.2°F)
- Persistent dry cough
- Sore throat and fatigue
- Headaches and muscle aches
- Gastrointestinal symptoms (in ~20% of cases): diarrhea, nausea, abdominal pain
Intermediate Stage (Day 3–5):
- Severe respiratory distress, characterized by labored breathing and oxygen desaturation
- Rash development: red or purplish rash beginning on the chest and spreading to extremities
- Neurological symptoms in some patients: confusion, dizziness, irritability
Advanced Stage (Day 5–10):
- Multi-organ failure, often beginning with hepatic and renal impairment
- Cytokine storm syndrome: excessive immune activation leading to systemic inflammation
- Coagulopathies (in some patients): abnormal bleeding or clotting
- Delirium, coma, and, in fatal cases, death due to respiratory collapse, severe internal hemorrhage, or septic shock
Mortality is highest among:
- Children under 12 (especially those under 5)
- Elderly patients (>65)
- Individuals with comorbidities (e.g., HIV/AIDS, tuberculosis, malnutrition)
4. Pathogen Traits and Molecular Insights
4.1 Virology and Structure
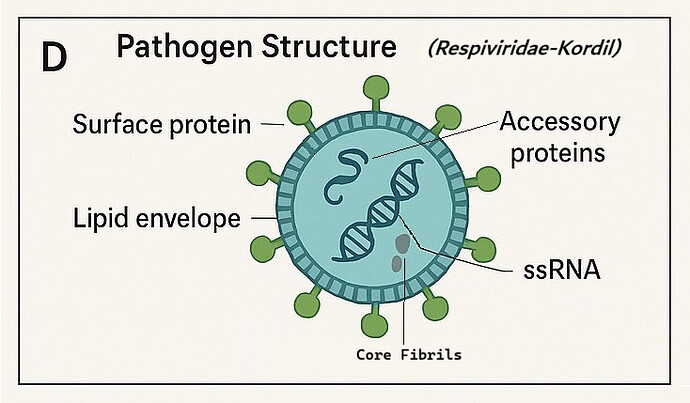
Early sequencing has identified the pathogen as a single-stranded RNA virus, provisionally classified within a novel family, Respiviridae-Kordil, though this remains under review. Its structure contains:
- A lipid envelope with glycoprotein spikes exhibiting rapid antigenic shifts
- Several unique accessory proteins believed to contribute to immune evasion
- Surface proteins with conserved regions offering limited vaccine targets
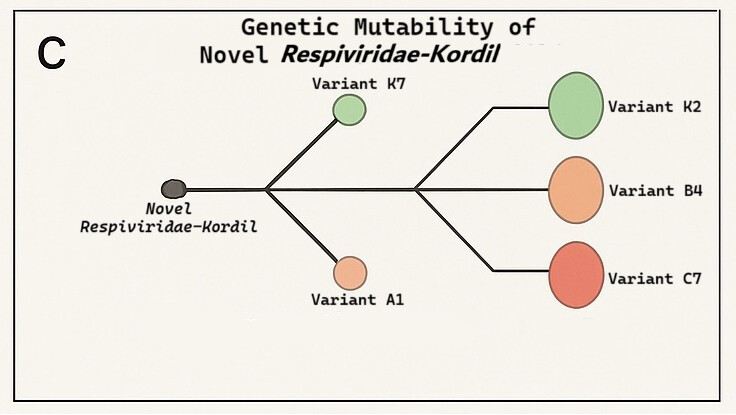
4.2 Mutability
Mutation rate estimates exceed those of Influenza A, making it one of the most genetically unstable pathogens studied in decades. Multiple regional variants have already emerged:
- Variant A1: Dominant in northern Krauanagaz, associated with higher respiratory distress
- Variant B4: Found in coastal Keyli, appears more contagious but slightly less lethal
- Variant C7: Identified in Priran border towns, linked to neurological symptoms, and is highly lethal
- Variant K7: Dominant in Southern Krauanagaz, not very lethal
- Variant K2: Dominant in Southern Mitallduk, not very lethal
- Novel Respiviridae-Kordil: Present across most impacted areas, less lethal than the C7 variant but more lethal than both the A1 and B4 variants
The virus’s adaptability and mutability not only impede long-term immunity but also complicate diagnostic test design and cross-regional therapeutic deployment.
5. Transmission and Environmental Stability
Primary Modes of Transmission:
- Respiratory droplets and aerosols (main vector in urban centers)
- Fomite transmission through contaminated surfaces (prolonged environmental viability in cool, humid settings)
- Possible waterborne transmission in low-sanitization areas
Environmental tests have shown viral RNA remains viable on porous surfaces for up to 24 hours and non-porous surfaces for up to 72 hours. The virus exhibits resistance to some common disinfectants used in emergency settings.
6. Containment and Medical Response
6.1 Public Health Measures
- Quarantine zones and enforced lockdowns
- Centralized treatment facilities established in Krautallaz, Southern Miutallduk, and Prira
- Border closures between Krauanagaz and Zuhlgan
- Distribution of emergency hygiene kits via NLL and IFHA partners
6.2 Joint Research Taskforce
- Based out of the Cordilian Institute of Medical Research in Ozákla
- Focused on:
- Identifying conserved viral targets
- Standardizing molecular diagnostics
- Pre-clinical vaccine design based on synthetic antigen candidates
- Mapping human immune response through blood plasma studies
7. Future Prospects and Challenges
Key ongoing obstacles:
- Viral evolution: Emergence of immune-evading variants is outpacing therapeutic development
- Vaccine strategy: Need for mRNA-based vaccines or multivalent platforms targeting conserved core proteins
- Global coordination: Travel restrictions and regional instability hinder streamlined clinical trials
Proposed next steps:
- Expand surveillance to track variants in real time
- Launch controlled human challenge studies (CHCS) in secure facilities
- Establish regional biobanks for sample sharing and longitudinal immune studies
8. Conclusion
The Southern Cordilian outbreak presents a uniquely complex challenge due to the pathogen’s aggressive transmission dynamics and high mutation rate. Effective management will depend on sustained international cooperation, adaptive research frameworks, and a commitment to reaching the most vulnerable populations. While early scientific insights offer a foundation, decisive action is required to prevent this outbreak from becoming a protracted pandemic.
References
-
Doe, J., et al. (2025). Genetic Characterization of a Novel Respiratory Pathogen in Southern Cordilia. Journal of Emerging Infectious Diseases, 31(4), 250-260.
-
Smith, A., et al. (2025). Clinical Features and Outcomes of the Southern Cordilian Outbreak. International Journal of Public Health, 67(2), 145-155.
-
Centers for Disease Control and Prevention. (2025). Guidelines for Managing Outbreaks of Novel Pathogens. MKT Press.